Mobile Stroke Units
MSUs are specialized ambulances equipped with CT scanner, laboratory equipment and telehealth connection. They are clinically operated through various staffing models under the clinical care of a stroke neurology physician in person or by telemedicine, a critical care or emergency medicine nurse, CT technologist and an Emergency Medical Services (EMS) paramedic. By bringing the hospital to the patient, MSUs expedite the conclusive diagnosis and treatment of stroke and have helped patients preserve quality of life after stroke.
NEUROMERIT CAN HELP ACTUALIZE AN MSU IN YOUR SYSTEM OF CARE
NeuroMerit provides expert consultation to guide your team in understanding how to build an MSU in your local community. This guidance includes detailed plans for rig build and design, hardware/software needs, clinical staffing models adaptable to your system of care, protocols for clinical operations, budget preparation and cost analysis, survey of plans for integration into local EMS/Fire Department systems of care, on site training of paramedics, nurses, CT technologists, physicians and all other team members involved.
Mobile Stroke Units
MSUs are specialized ambulances equipped with CT scanner, laboratory equipment and telehealth connection. They are clinically operated through various staffing models under the clinical care of a stroke neurology physician in person or by telemedicine, a critical care or emergency medicine nurse, CT technologist and an Emergency Medical Services (EMS) paramedic. By bringing the hospital to the patient, MSUs expedite the conclusive diagnosis and treatment of stroke and have helped patients preserve quality of life after stroke.
NeuroMerit Can Help Actualize an MSU in Your System of Care
NeuroMerit provides expert consultation to guide your team in understanding how to build an MSU in your local community. This guidance includes detailed plans for rig build and design, hardware/software needs, clinical staffing models adaptable to your system of care, protocols for clinical operations, budget preparation and cost analysis, survey of plans for integration into local EMS/Fire Department systems of care, on site training of paramedics, nurses, CT technologists, physicians and all other team members involved.
Recent Select Publications
Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: a randomised controlled trial
Abstract Background: Only 2-5% of patients who have a stroke receive thrombolytic treatment, mainly because of delay in reaching the hospital. We aimed to assess the efficacy of a new approach of diagnosis and treatment starting at the emergency site, rather than...
Mobile stroke units for prehospital thrombolysis, triage, and beyond: benefits and challenges
Abstract In acute stroke management, time is brain. Bringing swift treatment to the patient, instead of the conventional approach of awaiting the patient's arrival at the hospital for treatment, is a potential strategy to improve clinical outcomes after stroke. This...
Mobile stroke unit use for prehospital stroke treatment-an update
Abstract Background: Acute ischemic stroke is a treatable disease. Moreover, there is increasing evidence supporting mechanical recanalization for large-vessel occlusion, even beyond a strict time window. However, only small numbers of patients receive causal...
Melbourne Mobile Stroke Unit and Reperfusion Therapy: Greater Clinical Impact of Thrombectomy Than Thrombolysis
Abstract Background and Purpose- Mobile stroke units (MSUs) are increasingly used worldwide to provide prehospital triage and treatment. The benefits of MSUs in giving earlier thrombolysis have been well established, but the impacts of MSUs on endovascular...
Bringing Emergency Neurology to Ambulances: Mobile Stroke Unit
Abstract Ischemic stroke results from blocked arteries in the brain, with earlier thrombolysis with intravenous tissue plasminogen activator (tPA) and/or mechanical thrombectomy resulting in improved clinical outcomes. Mobile Stroke Unit (MSU) can speed up the...
Mobile Stroke Unit Computed Tomography Angiography Substantially Shortens Door-to-Puncture Time
Abstract Background and Purpose- Endovascular thrombectomy (ET) door-to-puncture time (DTPT) is a modifiable metric. One of the most important, yet time-consuming steps, is documentation of large vessel occlusion by computed tomography angiography (CTA). We...
Prehospital Stroke Management Optimized by Use of Clinical Scoring vs Mobile Stroke Unit for Triage of Patients With Stroke: A Randomized Clinical Trial
Abstract Importance: Transferring patients with large-vessel occlusion (LVO) or intracranial hemorrhage (ICH) to hospitals not providing interventional treatment options is an unresolved medical problem. Objective: To determine how optimized prehospital management...
Association Between Dispatch of Mobile Stroke Units and Functional Outcomes Among Patients With Acute Ischemic Stroke in Berlin
Abstract Importance: Effects of thrombolysis in acute ischemic stroke are time-dependent. Ambulances that can administer thrombolysis (mobile stroke units [MSUs]) before arriving at the hospital have been shown to reduce time to treatment. Objective: To determine...
MSU in the News
Use of mobile stroke units improves clinical outcomes
IMAGE: Berlin currently has three STEMOs, mobile stroke units which help reduce time to treatment. view more STEMOs (Stroke-Einsatz-Mobile) have been serving Berlin for ten years. The specialized stroke emergency response vehicles allow physicians to start treating...
UCLA Mobile Stroke Unit saves time, provides lifesaving care on the scene
The UCLA Mobile Stroke Unit is working to improve care for stroke victims by reducing the time between diagnosis and treatment. (Noah Danesh/Daily Bruin) Correction: The original version of this article incorrectly stated Soumya Ravichandran is a fourth-year student....
Direct Transfer to Angio Improves Outcome in Large-Vessel Stroke
Patient with suspected large-vessel occlusion stroke who were taken directly to the angiography suite, bypassing the emergency department, received endovascular treatment faster and had better 90-day functional outcomes in a new study. Results of the ANGIO-CAT trial...
Mobile stroke units deliver faster care to improve outcomes, lessen chance for disability
A new study involving UCLA researchers finds that mobile stroke units (MSUs) - state-of-the-art ambulances built to provide stroke patients with emergency neurological diagnosis and treatment prior to hospital arrival -- improve patient outcomes and lessen the chance...
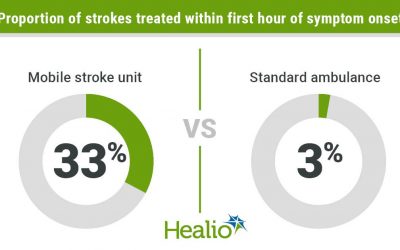
Management by mobile stroke unit led to better functional outcomes vs. standard ambulance
Patients who experienced a stroke and were treated by a mobile stroke unit were more likely to be treated within the first hour of symptom onset and more likely to be disability free at 90 days, a researcher reported. According to data from the BEST-MSU trial...
Mobile stroke units improve outcomes and reduce disability among stroke patients
DALLAS, March 17, 2021 -- Stroke patients treated via a mobile stroke unit (MSU) received clot-busting medications faster and more often - and recovered significantly better than patients who receive regular emergency care by standard ambulance, according to...
Mobile Stroke Units Improve Outcomes in Ischemic Stroke
Among patients with acute ischemic stroke, treatment in a mobile stroke unit (MSU) is associated with better functional outcome at 90 days, compared with standard management by emergency medical services (EMS). Click here to view original web page at...
Mobile Stroke Units Help Buy Valuable Minutes for the Damaged Brain
Credit: F. Muhammad/ Pixabay A new study involving UCLA researchers finds that mobile stroke units (MSUs) – state-of-the-art ambulances built to provide stroke patients with emergency neurological diagnosis and treatment prior to hospital arrival -- improve patient...
CONSULTANTS

MAY NOUR, MD, PHD
INTERVENTIONAL NEUROLOGIST
Dr. Nour is a dually trained vascular and interventional neurologist, completing her training at the University of California, Los Angeles (UCLA). She earned her medical degree (MD) from the University of Arizona College of Medicine and her doctorate degree (PhD) in neurosciences from the University of Oklahoma Center for Neurosciences. As medical director of California’s first mobile stroke unit which began clinical operations in 2017, Dr. Nour has extensive, first hand experience in initiation of mobile stroke programs and concrete knowledge of rig build and design, hardware/software integration, models for effective clinical staffing, clinical operating procedures, integration into EMS systems of care, budget/cost analysis and QI/QA for these specialized ambulance programs which bring the hospital to the patient. As a PI, Co-PI and Investigator for multiple clinical trials in the fields of vascular neurology and neurointervention, Dr. Nour has extensive experience in telehealth applications, clinical trial design, assessment and outcome analysis. Dr. Nour is currently an assistant professor of neurology and radiology at the University of California, Los Angeles.

KEVIN BROWN, RT (R) (CT)
CT TECHNOLOGIST
Mr. Brown is a registered CT technologist with over 10 years of experience in the field of radiologic imaging. Trained at the School of Radiologic Technology in Palm Beach County, his expertise spans fluoroscopy, x-ray, and multimodal CT imaging. Since 2017, Mr. Brown has been an integral part of the UCLA Health Mobile Stroke Unit team. He currently serves as the program manager of this specialized prehospital program and leads a diverse team of medical professionals. With an extensive background of work experience in healthcare, computing hardware/software, data management and team building, he understands the needs of the future healthcare evolution in prehospital management. With a firm belief in developing strong relationships and personal accountability, he is determined to achieve success through hard work and collegiality. He has experience in clinical research and is a contributing member of the BEST-MSU study. By attending national conferences in stroke care he continues to learn and meet with today’s innovators to improve the systems of care of which he is a part.
CONSULTANTS

May Nour, MD, PhD
Interventional Neurologist
SEE BIO

Kevin Brown, RT (R) (CT)
CT technologist
SEE BIO
May Nour, MD, PhD
Kenny Harrell
Firefighter paramedic Harrell has 15 years of experience as a firefighter for multiple fire department agencies. He has received extensive training in the specialties of Paramedicine, Hazardous Materials, and Aircraft Rescue Response. His experiences have fortified his base of knowledge as he advanced in his career with courage and leadership. Harrell served as the primary operator/paramedic of California’s first Mobile Stroke Unit from 2017-2020. Operationalizing the program from an EMS perspective as it evolved from a one to six fire department partnership and shared regional resource of Los Angeles County, he has served to support the growth of the program and training of its paramedic operators. Firefighter paramedic Harrell has served as a firefighter with the Santa Monica Fire Department since 2011 where he has promoted himself into a position of respect through the ranks, has written multiple policies for a variety of different responses and mentored several firefighters who have gone on to equally excel in their careers.
Kevin Brown, RT (R) (CT)
Mr. Brown is a registered CT technologist with over 10 years of experience in the field of radiologic imaging. Trained at the School of Radiologic Technology in Palm Beach County, his expertise spans fluoroscopy, x-ray, and multimodal CT imaging. Since 2017, Mr. Brown has been an integral part of the UCLA Health Mobile Stroke Unit team. He currently serves as the program manager of this specialized prehospital program and leads a diverse team of medical professionals. With an extensive background of work experience in healthcare, computing hardware/software, data management and team building, he understands the needs of the future healthcare evolution in prehospital management. With a firm belief in developing strong relationships and personal accountability, he is determined to achieve success through hard work and collegiality. He has experience in clinical research and is a contributing member of the BEST-MSU study. By attending national conferences in stroke care he continues to learn and meet with today’s innovators to improve the systems of care of which he is a part.

Contact NeuroMerit
Use the form below to contact the NeuroMerit Company, schedule a consultation or request general information about our services.

Phone
(424) 259-1233
info@neuromerit.com
HEADQUARTERS
Los Angeles, CA